- News & Events
- >news
Comparison with Tympanic Temperature in Stroke patients
A comparison of tympanic with core body temperature in stroke patients was performed by Ajčević et al. (2022) and reported in the Sensors journal. This work highlights the potential of core body temperature monitoring performed with greenteg’s technology as a method to track reliably stroke patients body temperature compared to standard temperature measurements.
A complete investigation of tympanic vs. core body temperature in Stroke patients
Research summary
About the difficulty of body temperature monitoring
An increase in temperature detected for patients admitted with stroke is associated with clinical worsening and increased mortality.
However, for stroke patients, the continuous monitoring of body temperature is important but difficult due to peripheral temperature measurements. Consequently, a continuous remote and non-invasive body temperature monitoring on body parts such as the chest, the upper-arm or the wrist could present an interesting alternative.
Core body temperature for patient monitoring
Body temperature monitoring helps health professionals’ decision-making and diagnostics. Core body temperature is among the physiological parameters commonly monitored in clinical studies. greenteg offers the world’s first core body temperature sensor for continuous and non-invasive measurements. The combination of our miniaturized sensor and AI-based algorithms are the backbone of our technology.
This technology currently supports three sensing solutions based on your application needs. The wearable core body temperature sensing solutions are described in details here. In addition, greenteg’s technology has been successfully employed in various clinical studies.
Core body temperature in stroke patients
The CALERA® solution was validated with CORE in an independent clinical study led by Miloš Ajčević, Alex Stella and co-workers at the Cattinara University Hospital ASUGI in Trieste, Italy. The study was performed on 30 partially febrile stroke patients over 6 months.
The study showed a good agreement of the CORE with commonly used tympanic ear temperature measurements with no bias and a Limit of Agreement of: LoA 95% CI −0.55 – 0.77 °C. The CORE measured effectively and accurately fever which is crucial for early detection of the deterioration of stroke patients. The detection was performed correctly in 94% of the cases. Hyperthermia and fever were defined respectively for temperatures above 37.5°C and 38.3°C.
In addition, the researchers compared greenteg’s sensor to a forehead thermometer commonly employed for the observation of Stroke patients. The forehead thermometer shows a proportional bias of -0.388°C and a 95% LoA of−0.72 – 1.00 °C with a trend of an overestimation of lower temperatures and an underestimation of higher temperatures.
The following graph represents the accuracy (LoA) of the CALERA® solution determined for this specific study in comparison with other clinical thermometers.
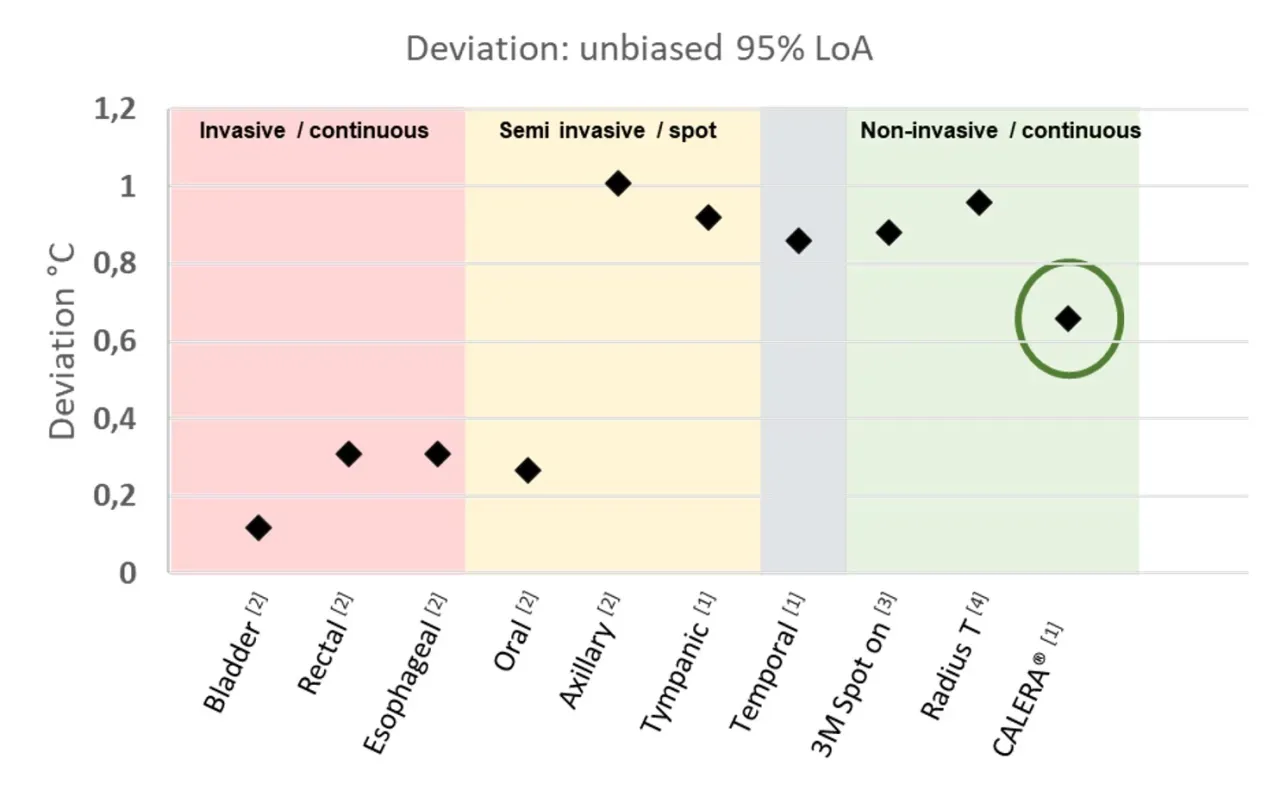
The corresponding exact values and references are given in the Table 1 below:
| Comparison of clinical thermometers | Bias (°C) | 95% LoA (°C) |
|---|---|---|
| Bladder[2] | 0.003 | 0.12 |
| Rectal[2] | 0.1 | 0.31 |
| Esophageal[2] | 0.003 | 0.31 |
| Oral[2] | 0.02 | 0.265 |
| Axillary[2] | -0.6 | 1.01 |
| Tympanic[1] | -0.03 | 0.92 |
| Temporal Artery[1] | 0.38 | 0.86 |
| SpotOn[3] | 0.23 | 0.88 |
| Radiuse T°[4] | 0.17 | 0.96 |
| CALERA[1] | 0.003 | 0.66 |
Conclusion
All in all, this study demonstrated that core body temperature monitoring performed with greenteg’s technology is a reliable alternative method for assessing core temperature in acute ischemic stroke patients compared to standard tympanic temperature measurements. Contact us for more information.
References
[1] Ajčević, Miloš, et al. “A Novel Non-Invasive Thermometer for Continuous Core Body Temperature: Comparison with Tympanic Temperature in an Acute Stroke Clinical Setting.” Sensors 22.13 (2022): 4760.
[2] Niven, Daniel J., et al. “Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis.” Annals of internal medicine 163.10 (2015): 768-777.
[3] https://multimedia.3m.com/mws/media/878163O/spoton-system-brochure.pdf
[4]https://usermanual.wiki/m/571d7c802c431cc72f88033bb1046c62ea38d64fbaf28d2f38bb09649a3067a8.pdf
